According to the World Health Organization (WHO) 2020 report, glaucoma is the most common cause of irreversible blindness worldwide after cataracts. Experts call it a “silent thief of sight,” as it causes permanent loss without the person’s knowledge. Until 2019, the global burden of glaucoma was around 79.6 million, with 50% affecting the Asian population. Affecting approximately 11.9 million Indians, blindness due to glaucoma is a growing cause of concern. The changes in the eye causing blindness due to glaucoma are slow, and most patients remain unaware of the underlying conditions.
Brief Explanation of Glaucoma
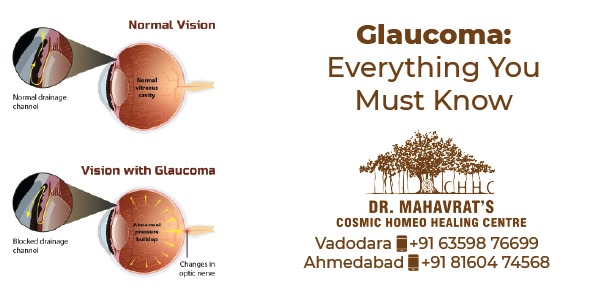
A glaucoma is a group of eye diseases that cause damage to the optic nerve (that supplies visual information to your brain from your eyes), eventually leading to blindness. Experts state that the damage is due to an increase in inter-eye pressures. The condition causes fluid to build up in the front part of the eye. This extra fluid increases the eye pressure, damaging the optic nerve. If it’s diagnosed early, you may be able to prevent additional vision loss. Glaucoma is usually, but not always, the result of abnormally high pressure inside your eye. Over the period of time, the increased pressure can erode your optic nerve tissue, which may lead to vision loss or even blindness.
How Glaucoma develops
The back of the human eye continuously makes a clear fluid called aqueous humor. As this fluid is made, it fills the front part of your eye. Then, it leaves the eye through channels in the cornea and iris. If these channels are blocked or partially obstructed due to any reason, the aqueous humor gets collected and natural pressure in your eye, which is called the intraocular pressure (IOP), increases. As IOP increases, the optic nerve may become damaged. As damage to the nerve progresses, the patient may begin losing sight in the affected eye.
Types of Glaucoma
1. Primary Open-Angle Glaucoma (Chronic Type)
The most common type of glaucoma gradually occurs when, in spite of having no abnormality in the drain structure (Trabecular Meshwork) of the eye, it fails to drain out fluid normally. The presence of extra fluid creates eye pressure, thereby damaging the optic nerve, this Damage is slow and painless. Generally, the primary open-angle glaucoma gives no warning signs in its early stages. Most people with this type of glaucoma fail to notice any change in their vision unless the damage is quite severe.
2. Pigmentary Glaucoma: This is a type of open-angle glaucoma that typically develops during early or middle adulthood. It involves changes in the pigment cells that give color to the iris. In pigmentary glaucoma, the pigment cells disperse throughout the eye. If the cells build up in the channels that drain fluid from the eye, they can upset the normal flow of fluids in the eye. This can lead to a rise in eye pressure
3. Angle-Closure Glaucoma (Acute Type)
Also referred to as closed-angle glaucoma or narrow-angle glaucoma, that occurs when there is narrowing/ blockage of drainage angle and there is a huge collection of aqueous humor. The drain space between the iris and cornea becomes too narrow. This can cause a severe, quick, painful, and sudden build-up of pressure in the eye. Patients with this type of glaucoma experience sudden blurry vision and severe eye pain with headaches and vomiting. Experts refer to it as an acute attack. It is an emergency that, if not treated, might cause vision loss in patients.
4. Congenital Glaucoma
Very rarely few children are born with the improper formation of drainage canals, such patients have a defect in the angle of their eye, which slows or prevents normal fluid drainage, and they develop congenital glaucoma. Congenital glaucoma usually presents with symptoms, such as cloudy eyes, excessive tearing, or sensitivity to light. Congenital glaucoma can run in families.
5. Normal-Tension Glaucoma
In some cases, people without increased eye pressure develop damage to their optic nerve. The cause of this isn’t known. However, extreme sensitivity or reduced blood flow (as a result of a condition such as atherosclerosis- a hardening of the arteries) to the optic nerve may be a factor in this type of glaucoma.
6. Secondary Glaucoma
Develops as a result of eye injury/ cataract/ eye tumor/ diabetes or sometimes long-term usage of corticosteroids may also lead to this condition.
Causes and Risk Factors of Glaucoma
Risk factors for developing glaucoma include:
- Patients over the age of 40 (in black and Hispanic people) and 60 (in American people)
- Family history of glaucoma
- Having Diabetes Mellitus, high blood pressure, heart disease, or sickle cell anemia.
- Farsighted and nearsighted patients (Myopia)
- Patients having an eye injury
- Long-term consumption of some medicines such as corticosteroids/ medicines for seizures/ some over-the-counter cold medicines.
- Having a cornea that is thinner than usual at the center
- Thinning of the optic nerve
People suffer from chronic diseases, including diabetes, migraine, hypertension, poor blood circulation, and other health problems.
Diagnosis of Glaucoma: Ophthalmologists perform a comprehensive eye examination that evaluates whether a patient has the risk of developing glaucoma. Besides, an ophthalmologist might also recommend special tests, such as visual field testing, optical coherence tomography, pachymetry, gonioscopy, visual evoked potential, and anterior segment OCT for detecting glaucoma. To diagnose glaucoma, ophthalmologists may also use one or more of the following tests and procedures:
- Detailed Medical History
Your doctor will want to know what symptoms you’ve been experiencing and if you have any personal or family history of glaucoma. They’ll also ask for a general health assessment to determine if any other health conditions may be impacting your eye health, such as diabetes or high blood pressure.
- Tonometry Test
The most crucial test is checking the eye pressure performed with a tonometer. The tonometer touches the surface of the eye. Some ophthalmologists use a “non-contact” tonometer with a gentle puff of air to read the internal eye pressure.
- Pachymetry Test
People with thin corneas have an increased risk of developing glaucoma. A pachymetry test can tell your doctor if your corneas are thinner than average.
- Perimetry Test
This test, also known as a visual field test, can tell your doctor if glaucoma is affecting your vision by measuring your peripheral, side, vision, and central vision.
- Monitoring Your Optic Nerve
If the doctor wants to monitor for gradual changes to your optic nerve, they may take photographs of your optic nerve to conduct a side-by-side comparison over time.
Why Choose Cosmic Homeo Healing Centre?
Cosmic Homeo Healing Centre is an established homeopathic treatment center operating for over seven decades with clinical case records of the same timeline. Along with the conventional treatment, Homeopathic Remedies have proved to be effective in controlling the eye pressure consistently and preventing further vision loss, which is again confirmed by the perimetry test (Visual Field Test) of the affected eye. Here are a few Homeopathic medicines mentioned that are proven effective in glaucoma treatment:
- Phosphorus: This remedy is useful to improve the vision of the affected eye, and also prevents further damage to the optic nerve. The patient experiences foggy vision as if he/ she is seeing through mist/ dust.
- Saponaria: This remedy is indicated when there is high intraocular pressure and the patient feels violent stitches deep inside the eyes. Saponaria helps to reduce elevated intraocular pressure.
- Phytolacca: Helps to improve the dim vision of the eye with dull aching pain deep inside the eye.
- Rhododendron: This medicine is useful in the developing stage of glaucoma where the patient does not have constant pain, but it comes and goes. Eyepains are mainly felt before thunderstorms.
- Few other medicines worth mentioning here are Gelsemium, Bryonia, Prunus Spinosa, Spigelia, Conium, etc.